Abstract
Background: We provided a comparative presentation of complications seen in 114 patients with port catheter implantation. In addition, we addressed whether patients with catheter-related thrombosis have distinctive features by assessing patients who developed thrombosis either at the catheter implant site or vascular bed.
Methods: In this study, we analyzed data from 114 patients who underwent subclavian venous port catheter implantation by a single surgeon at Kayseri Teaching Hospital (Turkey) during 2013 to 2016. Subclavian port catheter was inserted in all cases. The diagnosis of port thrombosis was made by Doppler sonography or thorax CT scan with contrast enhancement in patients presenting with edema at upper extremity, swelling or pain at neck, and/or dysfunctional port.
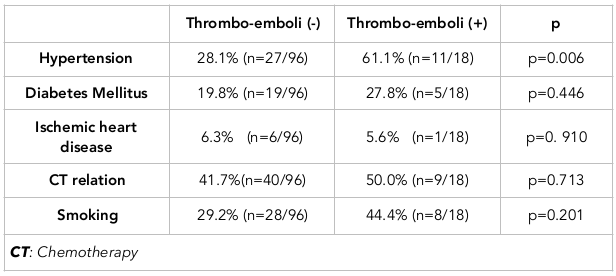
Results: Seroma was detected in only one case, lymphedema developed in one case (0.8%), and pneumothorax was observed in 3 cases. The subclavian vein was implanted on the right side in all patients with pneumothorax. None of these cases were associated with thrombosis. Port infection was observed in one case (0.8%). There was also one case (0.8%) of skin necrosis. The port was removed in 15 patients due to several reasons, which are indicated in Table 2. Thromboembolic events were observed in 11 of the 114 patients while port thrombosis was observed in 7 patients. The rate of hypertension in the thromboembolism group was 61.1% (11/18 individual) while the rate of hypertension in the group without thromboembolism was 28.1% (27/96 individuals); this difference was statistically significant (p = 0.006).
Conclusion: In this study, based on complications observed in patients with catheter-related thrombosis, factors such as smoking or diabetes mellitus were seen to be linked to thromboembolism and should be taken into consideration. Moreover, it was observed that hypertension had a significant association with thromboembolism.
Introduction
Venous ports were first introduced by Niederberhuber et al. in 1982 Niederhuber et al., 1982. Venous port systems are used to administer chemotherapy in oncology. In addition, they may also be used for volume replacement, detoxification, blood and blood product transfusion, intravenous infusion of sclerosing agents, other drug infusions, parenteral nutrition, laboratory follow-up, and diagnostic purposes Biffi et al., 2009Esfahani et al., 2016Ignatov et al., 2009. Moreover, in oncology practice over the past two decades, patients requiring prolonged treatment with chemotherapeutic agents are thought to benefit most from subcutaneous venous port catheters.
The catheters provide long-term parenteral nutrition in patients with problems in feeding. Additionally, the catheters prevent trauma and contribute to comfort in patients requiring periodical blood sampling. They also have other advantages such as enabling sclerosing agent infusion and facilitating fluid replacement. Port catheters are more advantageous, both aesthetically and functionally, than catheters with tip over skin, as they are inserted subcutaneously and have reduced risk of infection.
Besides the aforementioned advantages, complications may occur either during implantation or use of these catheters. Indeed, adverse events from use of the catheters have been reported in the literature. Early complications include bleeding or pneumothorax related to catheter implantation; long-term complications include infections. Thrombosis can develop as a complication in oncologic patients and in non-oncology patients.
Thrombosis has often been studied to explore predictive markers and to identify risk factors Erden et al., 2017aErden et al., 2017b. There have also been many efforts to prevent thrombosis. Although flushing with heparin solution is routinely employed, its role is controversial in the prophylaxis of thrombosis Cesaro et al., 2009Stephens et al., 1997. Moreover, the incidence of thrombosis caused by central venous catheterization is markedly high.
Many researchers have published about their experiences of the use of subcutaneous venous port catheters over time. In our study, only subclavian catheters were taken into consideration. In this study, we provide a comparative presentation of complications seen in the study including 114 patients. In addition, we addressed whether patients with catheter-related thrombosis have distinctive features by assessing patients who developed thrombosis either at the catheter or vascular bed.
Materials - Methods
In this study, we analyzed data from all of the 114 patients who had undergone subclavian venous port catheter implantation by a single surgeon at Kayseri Teaching Hospital between 2013 and 2016. This study was approved by the Kayseri Training and Research Hospital Ethics Committee.
Port catheter implantation
Patients who were recommended to receive chemotherapy were referred to our clinic. All port catheter implantations were performed at the operating theatre under regional anesthesia with standard monitoring. No antibiotic prophylaxis was employed. In all patients, an 8.5 Fr single-lumen port catheter was used. The right subclavian vein was preferred as the catheterization site in most cases. However, the left subclavian vein was used if the right subclavian vein was ineligible due to previous mastectomy or radiation scars.
Prior to catheter implant, a 0.5 cm skin incision was made just below the clavicle. The subclavian vein was punctured by using a 10-ml syringe and 18G needle. After venous puncture, the guidewire was advanced to superior vena cava. Then, the needle was pulled back, and peel-away was inserted into subclavian through guidewire. When peel-away was in place, the guidewire was pulled back and the catheter was advanced to vena cava superior within peel-away.
To place the port, a subcutaneous pocket was created over pectoral muscle at midline via a 3-cm skin incision. In order to connect the catheter, a trocar was inserted from the skin incision at the clavicle and advanced to pockets created over pectoral muscle. Then the distal end of the catheter was connected to the port. Blood aspiration was performed by using a port needle. Following confirmation, the port catheter was flushed by normal saline and the reservoir was filled with diluted heparin (2500 U standard heparin in 100 cc normal saline). The port was fixed to fascia of pectoral muscle and the tissues were closed in standard fashion. In all patients, a chest radiograph was obtained after to evaluate potential complications. The patient and his/her relatives were informed about port care and were instructed to flush the port by heparinized normal saline (500 U heparin in 10 cc normal saline) after each drug infusion. Skin sutures were removed on day 7. The patients were instructed to report and notify any problems associated with the port.
Diagnosis of thrombosis
The diagnosis of port thrombosis was made by Doppler sonography or thorax Computerized Tomography scan with contrast enhancement in patients presenting with edema at upper extremity, swelling or pain at neck, and/or dysfunctional port.
Statistical Analysis
The continuous data are presented as mean and standard deviation or median and percentiles. Student's t test was used to compare continuous variables between groups. Mann-Whitney U test was used to compare medians of numerical variables with skewed distribution. Chi-square test was used to compare categorical variables. Pearson correlation analysis was used to assess the relationship between patient and control groups. A p-value <0.05 was considered as significant. All statistical analyses were conducted using the SPSS version 21.0 statistical software (Statistical Package for Social Sciences; SPSS Inc., Chicago, Illinois).
Results
In this study, we used data from 114 patients who underwent subcutaneous port catheter implantation at the subclavian vein by a single cardiovascular surgeon for chemotherapeutic drug infusion.
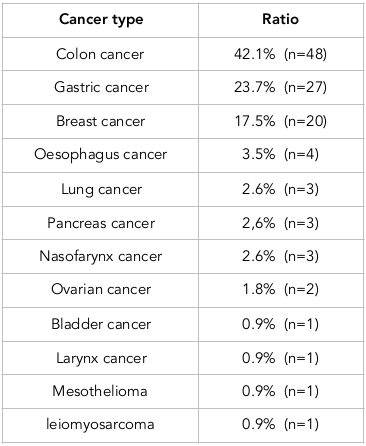
Of the patients who had undergone port implantation, 47.4% were male whereas 52.6% were female. The median age was 56 years (range: 21-82 years). The port was implanted into the right subclavian vein (96.5% of patients) and into the left subclavian vein (3.5% of patients). Table 1 shows the distribution of the underlying diseases of patients who underwent subclavian port implantation.
Seroma was detected in only one case. Lymphedema was also developed in one case (0.8%). Pneumothorax was observed in 3 cases. Subclavian vein was implanted to right side in all patients with pneumothorax. None of these cases were associated to thrombosis. Port infection was observed in once case (0.8%). There was also one case (0.8%) with skin necrosis.
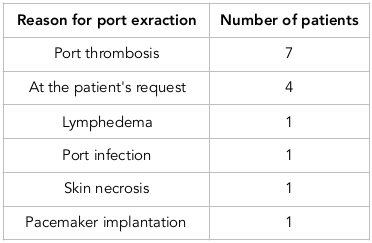
Subclavian port catheter was inserted in all cases. Port was removed in 15 patients due to several reasons. Table 2 presents reasons for port extraction. Port revision was needed in 2.6% of cases and was due to thrombosis at the reservoir and lumen (in 2 cases) and advancement at the jugular vein (in 1 case).
Port thrombosis
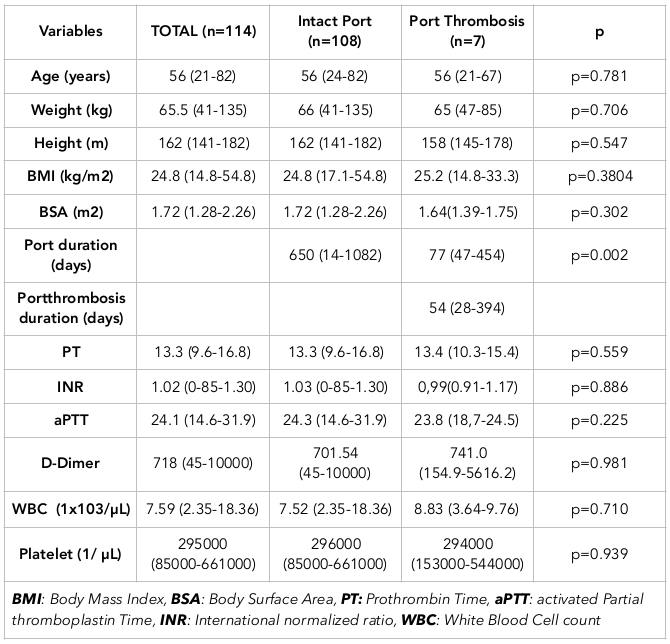
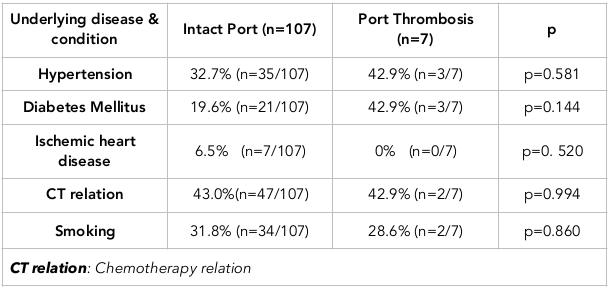
Port thrombosis was observed in 7 cases. The median time to thrombosis was 54 days (range: 28-394 days). Of 7 patients with port thrombosis, there was colon cancer in 3, breast cancer in 2, pancreas cancer in 1, and gastric carcinoma in 1 case. Table 3 presents comparisons between cases with or without port thrombosis. Table 4 represents the relationship of port thrombosis with underlying diseases or conditions.
Thromboembolism
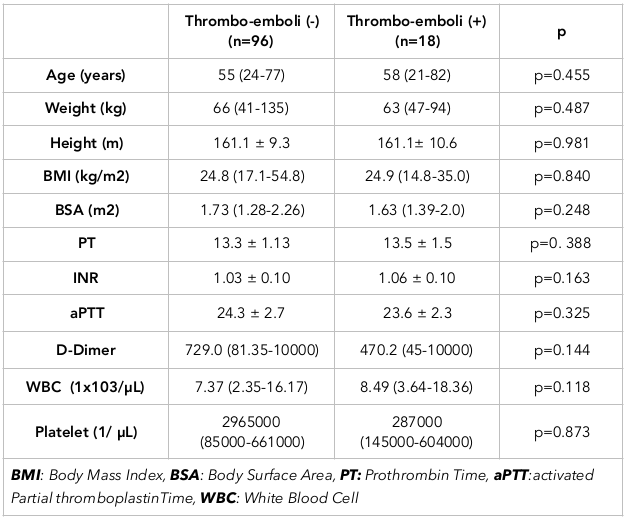
Thromboembolic events are observed in 11 of 114 patients, while port thrombosis was observed in 7 patients. Taken together, there was an thromboembolic event or port thrombosis in 18 patients, while there was no such complication in the remaining 96 patients. When these groups were compared, the age distribution was similar between the groups (p=0.455). Male:female distribution was 61.1%/38.9% in thrombosis/embolism group while it was 44.8%/55.2% in the group without thrombosis/embolism. There was no significant difference in gender between the groups (p=0.203). Table 5 presents comparison of groups. Table 6 presents the relationship of thrombosis/embolism with underlying diseases or conditions.
Discussion
More than two decades, port catheters have been used in oncology patients for its many benefits/advantages. However, port catheters may be associated with some undesired conditions, including thrombosis and peripheral embolism. In this study, we compared patients with thromboembolic complications to those without, and reviewed the complications for the study groups.
Despite advantages, several complications may occur during implantation or use of subclavian port catheters. Adverse events observed in our study are generally in agreement with the literature. The important aspect of our study was that a single surgeon performed the insertion of port catheters in 114 patients. With this method, standardization differences due to application were also avoided.
Pneumothorax: In the literature, pneumothorax rate has been reported as 0.1-3.2% Samanc et al., 2004. In our series, pneumothorax occurred in 2.6% (n=3) of patients.
Port catheter infection: In our series, port catheter infection was observed in only one patient. In the literature, port catheter infection rate varies from 0.8% to 7.5% Biffi et al., 2009Ignatov et al., 2009; Suslu et al., 2012. There is insufficient data to support benefit of antibiotic use before or after procedures.
Lymphedema: Lymphedema was developed in one patient (0.8% female) who underwent bilateral mastectomy and lymph node dissection. Given the lymphedema rate was reported as 3.6% in the literature, the lymphedema rate in our series could be considered as better Gandhi et al., 2003.
Port extraction: Port extraction was needed in 15 of 114 port catheters. The major cause for extraction was port catheter thrombosis; followed by patient's request. Table 2 presents reasons for port extraction.
Port revision: Port revision is required in 2.6% of all patients. Reasons for port revision include: thrombosis at reservoir and lumen in 2 patients and advancement of catheter to the jugular vein in one patient.
Skin infection: As a complication of port implantation, skin infection is reported in approximately 1% of cases. In agreement with the literature, skin infection was observed in only one patient (0.88%) in our series Aziret et al., 2015Cil et al., 2006; the patient received chemotherapy for breast cancer and had a BMI of 31.2 kg/m2.
Thrombosis: Thrombosis may develop during the early period but also may be delayed up to 161 days. Silicone catheters have relatively smoother surface and are less thrombogenic. Polyurethane or Teflon catheters are known to be more thrombogenic Morris et al., 1992. In our series, the median time to port catheter thrombosis was 54 days (ranging from 28 to 394 days). The median time was calculated by using data of 7 patients with port-catheter thrombosis and did not include cases with port-related venous thrombosis.
Body mass index (BMI) or body surface area (BSA): No significant difference was observed in thromboembolism between groups when BMI and BSA were assessed. However, skin infection was observed in a female patient with BMI of 31.2 kg/m2.
Chemotherapy: Although there was no marked relationship between thromboembolism and chemotherapeutic administration, the relationship tended to be stronger in the thromboembolism group ( Table 6 ).
Smoking: Although there was no significant difference, it was seen that there was tendency to thromboembolic events among smokers. Larger sample sizes may reveal a statistical significance.
Comorbid conditions: Comorbid conditions (including hypertension, diabetes mellitus, and ischemic heart disease) were also reviewed. No marked relationship was observed with ischemic heart disease since there was only one patient with ischemic heart disease in the thromboembolism group.
When diabetes mellitus was assessed, it was seen that the diabetes mellitus rate was higher in the thromboembolism group. This finding suggests that a significant relationship may be observed in a multi-center study with larger sample size. In our study, there was a significant difference in hypertension between groups.
Thromboembolism-hypertension: In this study, hypertension in patients had several components that were associated significantly to features of patients with thrombosis (as compared to those without). This difference was significant for both catheter thrombosis and catheter-related thrombosis.
It is thought that platelets and endothelium are activated during hypertension, resulting in predisposition to thrombosis. The damage caused by hypertension in vessels develops due to thrombotic complications rather than hemorrhage, resulting from increased pressure of hypertension Lip, 2000.
In Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT), Spencer et al. showed the presence of increased von Willebrand factor in patients with end-organ injury; however, they failed to establish a correlation between increased von Willebrand factor levels and platelet counts or p-selectin (a soluble adhesion molecule) Spencer et al., 2002.
It is known that vessel calibration and diameter are important risk factors for thrombosis Ogata et al., 2013. In a recent meta-analysis, it was suggested that hypertension might be a risk factor for deep vein thrombosis following orthopedic surgery Huang et al., 2016.
Hypertension is a risk factor linked to acute pulmonary embolism, as are diabetes mellitus, elevated serum cholesterol levels, and smoking Ageno et al., 2008. It is already known that hypertension leads to predisposition of thrombosis by causing atherosclerosis Chang-jun, 2013.
The diversity of cancer types, the lack of standardization of the stages of the patients, and the differentiation of comorbid diseases for each patient can be considered as limiting aspects of the study.
Conclusion
In our study, we reviewed adverse events, particularly thromboembolic events that are related to port catheters implanted into the subclavian vein. These events are the major causes warranting port catheter extraction. In this study, it was observed that factors such as smoking or diabetes mellitus should be taken into consideration regarding thromboembolism while hypertension had a significant association with thromboembolism. It may be advantageous to investigate port catheters implanted by single surgeon for standardization; however, a multicenter study with larger sample size will allow drawing more definitive conclusions.
Abbreviations
aPTT: activated Partial thromboplastin Time
BMI: Body Mass Index
BSA: Body Surface Area
CT relation: Chemotherapy relation
INR: International normalized ratio
PT: Prothrombin Time
WBC: White Blood Cell count
Author Contribution
Dr. Ruchan ANBAR: The surgeon who placed the port catheters in patients and text writing. Dr.Deniz AVCI: literature review, text writing and statistics. Dr. Ali CETINKAYA: literature review, text writing and statistics. All authors approved the final manuscript.
References
-
W.
Ageno,
C.
Becattini,
T.
Brighton,
R.
Selby,
P. W.
Kamphuisen.
Cardiovascular risk factors and venous thromboembolism: A meta-analysis. Circulation.
2008;
117(1)
:
93-102
.
View Article Google Scholar -
M.
Aziret,
O.
İrkörücü,
C.
Gökler,
E.
Reyhan,
S.
Çetinkünar,
T.
Çil.
Performance of venous port catheter insertion by a general surgeon: A prospective study. International Surgery.
2015;
100(5)
:
827-835
.
View Article Google Scholar -
R.
Biffi,
F.
Orsi,
S.
Pozzi,
U.
Pace,
G.
Bonomo,
L.
Monfardini,
A.
Goldhirsch.
Best choice of central venous insertion site for the prevention of catheter-related complications in adult patients who need cancer therapy: A randomized trial. Annals of Oncology : Official Journal of the European Society for Medical Oncology.
2009;
20(5)
:
935-940
.
View Article Google Scholar -
S.
Cesaro,
G.
Tridello,
M.
Cavaliere,
L.
Magagna,
P.
Gavin,
R.
Cusinato,
M.
Carli.
Prospective, randomized trial of two different modalities of flushing central venous catheters in pediatric patients with cancer. Journal of Clinical Oncology.
2009;
27(12)
:
2059-2065
.
View Article Google Scholar -
G.
Chang-jun.
Risk factors of deep venous thrombosis after traumatic fracture. J N Pharm.
2013;
8
:
99-100
.
-
B. E.
Cil,
M.
Canyiğit,
B.
Peynircioğlu,
T.
Hazirolan,
S.
Carkaci,
S.
Cekirge,
F.
Balkanci.
Subcutaneous venous port implantation in adult patients: A single center experience (PMID:16752357). Diagnostic and Interventional Radiology (Ankara, Turkey).
2006;
12(2)
:
93-98
.
-
F.
Erden,
H.
Karagoz,
A.
Avci,
D.
Avci,
A.
Cetinkaya,
S.
Bahadir,
A.
Erden.
Which one is best? platelet/lymphocyte ratio, neutrophil/lymphocyte ratio or both in determining deep venous thrombosis in behcet’s disease?. Biomedical Research.
2017a;
28
.
-
F.
Erden,
H.
Karagoz,
A.
Avci,
D.
Avci,
A.
Cetinkaya,
A.
Erden.
The values of mean platelet volume and the mean platelet volume/platelet ratio for predicting deep venous thrombosis in Behçet’s disease. LaboratoriumsMedizin-Journal of Laboratory Medicine.
2017b;
41
:
153-157
.
-
H.
Esfahani,
M.
Ghorbanpor,
A.
Tanasan.
Implantable Port Devices, Complications and outcome in Pediatric Cancer, a Retrospective Study (PMID:27222696). Iranian Journal of Pediatric Hematology and Oncology.
2016;
6(1)
:
1-8
.
-
R. T.
Gandhi,
G. I.
Getrajdman,
K. T.
Brown,
E. J.
Gandras,
A. M.
Covey,
L. A.
Brody.
Placement of subcutaneous chest wall ports ipsilateral to axillary lymph node dissection. Journal of Vascular and Interventional Radiology.
2003;
14(8)
:
1063-1065
.
View Article Google Scholar -
L.
Huang,
J.
Li,
Y.
Jiang.
Association between hypertension and deep vein thrombosis after orthopedic surgery: A meta-analysis. European Journal of Medical Research.
2016;
21(1)
:
13
.
View Article Google Scholar -
A.
Ignatov,
O.
Hoffman,
B.
Smith,
J.
Fahlke,
B.
Peters,
J.
Bischoff,
S. D.
Costa.
An 11-year retrospective study of totally implanted central venous access ports: Complications and patient satisfaction. European Journal of Surgical Oncology.
2009;
35(3)
:
241-246
.
View Article Google Scholar -
G. Y. H.
Lip.
Hypertension and the prothrombotic state. Journal of Human Hypertension.
2000;
14(10-11)
:
687-690
.
View Article Google Scholar -
S. L.
Morris,
P. F.
Jaques,
M. A.
Mauro.
Radiology-assisted placement of implantable subcutaneous infusion ports for long-term venous access. Radiology.
1992;
184(1)
:
149-151
.
View Article Google Scholar -
J. E.
Niederhuber,
W.
Ensminger,
J. W.
Gyves,
M.
Liepman,
K.
Doan,
E.
Cozzi.
Totally implanted venous and arterial access system to replace external catheters in cancer treatment (PMID:7123491). Surgery.
1982;
92(4)
:
706-712
.
-
T.
Ogata,
M.
Yasaka,
Y.
Wakugawa,
T.
Kitazono,
Y.
Okada.
Association of deep venous thrombosis with calf vein diameter in acute hemorrhagic stroke. Journal of Stroke and Cerebrovascular Diseases.
2013;
22(7)
:
1002-1005
.
View Article Google Scholar -
T.
Samanc,
N.
Molinas Mandel,
A.K.
Bozkurt,
F.
Kutlu,
C.
Uras.
Evaluation of port complications in 115 cancer patients. Cerrahpaşa J Med.
2004;
35
:
71-77
.
-
C. G.
Spencer,
D.
Gurney,
A. D.
Blann,
D. G.
Beevers,
G. Y. H.
Lip,
Anglo-Scandinavian Cardiac Outcomes Trial.
the ASCOT Steering Committee.
Von Willebrand factor, soluble P-selectin, and target organ damage in hypertension: A substudy of the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT). Hypertension.
2002;
40(1)
:
61-66
.
View Article Google Scholar -
L. C.
Stephens,
W. D.
Haire,
S.
Tarantolo,
E.
Reed,
K.
Schmit-Pokorny,
A.
Kessinger,
R.
Klein.
Normal saline versus heparin flush for maintaining central venous catheter patency during apheresis collection of peripheral blood stem cells (PBSC). Transfusion Science.
1997;
18(2)
:
187-193
.
View Article Google Scholar -
H.
Süslü,
G.
Arslan,
K.
Tural.
[Venous port implantation in adult patients: Retrospective evaluation]. The Journal of the Turkish Society of Algology.
2012;
24(1)
:
32-36
.
View Article Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 12 (2017)
Page No.: 1898-1910
Published on: 2017-12-29
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 28995 times
- Download PDF downloaded - 2355 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress