
Association of the International Academy of Cytology category with the Breast Imaging Reporting and Data System score in relation to the diagnostic accuracy for breast lumps
- Department of Pathology, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India
- Department of Radiodiagnosis, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India
- Department of Surgery, Sri Devaraj Urs Medical College, Sri Devaraj Urs Academy of Higher Education and Research, Kolar, Karnataka, India
Abstract
Background: Breast lumps are the commonest patient presentation in breast clinics. Initial diagnostic approaches, such as mammography and fine needle aspiration cytology (FNAC), help in prompting proper preoperative diagnosis and planning management.
Methods: This retrospective study included all patients who presented with breast lumps and underwent breast imaging (with Breast Imaging Reporting and Data System [BIRADS] scoring) and FNAC (with International Academy of Cytology [IAC] category assessment) in our hospital. The IAC category was compared with the BIRADS score. The FNAC and mammographic findings were compared with available histopathological findings. Data were entered into MS Excel worksheets, and statistical analysis was conducted using SPSS 22.0.
Results: A total of 60 patients were included in the study. The mean patient age was 40.11 years. Of the 60 cases, 35 benign cases and 15 malignant cases were concordant with the diagnosis according to the BIRADS score and IAC category. The association between the BIRADS score and IAC category was significant (p = 0.004). The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of the BIRADS score in diagnosing breast lesions were 85.37%, 78.95%, 89.74%, 71.43%, and 83.33%, respectively, compared with those of the IAC category. The sensitivity, specificity, PPV, NPV, and accuracy of the IAC category were 82.35%, 92.31%, 93.33%, 80.0%, and 86.67%, respectively, compared with those of the available histopathological findings. The sensitivity, specificity, PPV, NPV, and accuracy of the BIRADS score were 76.92%, 76.47%, 71.43%, 81.25%, and 76.67%, respectively, compared with those of the available histopathological findings.
Conclusion: FNAC with IAC category assessment and mammography with BIRADS scoring can be used as first-line diagnostic tests for breast lumps. However, FNAC is more sensitive in diagnosing breast lumps than mammography.
Introduction
Breast lumps are the commonest patient presentation in breast clinics1.The majority of breast lumps are eventually diagnosed as breast cancer. Hence, women with breast lumps must be appropriately evaluated and diagnosed, considering that breast cancer is the most common type of cancer in women worldwide and the most common cause of mortality among women with cancer1. In India, breast cancer is the second most common type of cancer in women. Further, its age-adjusted incidence in women is 25.8 per 100,000 individuals, and its mortality is 12.7 per 100,000 individuals. The incidence of breast cancer in Bangalore is 34.4%2, while the prevalence among women in Kolar is 6.4%3.
Considering the piteous state and significant mortality caused by breast cancer, especially in developing nations, the quality of evaluation by diagnostic services for breast cancer in women should be improved1. Accordingly, appropriate evaluation is required, including detailed history-taking, breast examination, imaging, and cytology/tissue diagnosis. Failure to perform such may lead to inappropriate treatment decisions4.
Although the final diagnosis is based on the histopathological findings of tissues, excision or biopsy of all breast lumps is not feasible. Hence, initial diagnostic approaches, such as mammography and fine needle aspiration, which are simple, rapid, presumptive, inexpensive, and safe methods, are important because they not only benefit both patients and clinicians by prompting proper preoperative diagnosis and management but also avoid unnecessary testing and procedures4.
The International Academy of Cytology (IAC) established a comprehensive and standardized approach to categorize the findings of fine needle aspiration cytology (FNAC) of breast lesions into C1 to C5. This structured reporting can improve the quality, reproducibility, and clarity of reports across departments/institutions as well as assist in patient management, improve breast health care, and facilitate further research.
The Breast Imaging Reporting and Data System (BIRADS) score was introduced by the American College of Radiologists for evaluating the findings of breast mammography to reduce inter-observer variability, standardize imaging reports, predict risks, and achieve verbal uniformity using well-defined and standard language. It can be utilized by radiologists, treating physicians, and surgeons, as it reflects the true nature of lesions, ultimately helping in specific diagnoses and treatment plans. However, the rate of false-negative cases based on mammographic findings of a palpable breast mass has been estimated between 4% and 12%5, 6, 7, 8. Therefore, malignancy cannot be excluded even when mammographic findings of a palpable mass suggest benign or borderline lesions.
In the present study, we evaluated the association of the IAC category on FNAC with the BIRADS score on mammography.
Methods
This retrospective study was conducted at the department of pathology of a tertiary health care center. Institutional ethical approval was obtained for the study. All patients who presented with breast lumps and underwent breast imaging (with BIRADS scoring in accordance with the latest guidelines) and FNAC were included in the study. Patients with recurrent breast cancer, non-cooperative patients, and pregnant and lactating patients were excluded from the study.
FNAC slides were retrieved from the cytology section of the department of pathology and screened by two pathologists. Any difference in the opinion of the two pathologists was discussed and resolved via consensus. All slides were categorized in accordance with the IAC guidelines as follows (C code): C1: insufficient material, C2: benign lesion, C3: atypical and probably benign, C4: suspicious and probably or invasive carcinoma, and C5: malignant. C1 to C3 were grouped as benign cases and C4 and C5 as malignant cases4.
The mammographic findings were scored using the BIRADS as follows: score 1: negative, score 2: benign, score 3: probably benign, score 4: suspicious for malignancy, score 4A: slightly suspicious for malignancy, score 4B: moderately suspicious for malignancy, score 4C: highly suspicious for malignancy, score 5: highly suggestive of malignancy, and score 6: known biopsy-proven malignancy9. Scores 1 to 3 were grouped as benign cases and scores 4 and 5 as malignant cases.
The FNAC and mammographic findings were compared with available histopathological findings. The IAC category was also compared with the BIRADS score. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of the IAC category and BIRADS score in diagnosing different breast diseases were calculated and analyzed in relation to the available histopathological findings.
Data were entered into MS Excel worksheets and analyzed using SPSS 22.0. Categorical data were presented as frequencies and proportions. The chi-square test was used for determining the significance of qualitative data. Continuous data were presented as means and standard deviations. P values of <0.05 were considered statistically significant. The sensitivity, specificity, PPV, NPV, and diagnostic accuracy were calculated.
Age distribution of breast lesions in the present study
|
Sl.No |
Age distribution |
No of cases |
|---|---|---|
|
1 |
10 - 19 |
5 |
|
2 |
20 - 29 |
12 |
|
3 |
30 - 39 |
13 |
|
4 |
40 - 49 |
15 |
|
5 |
50 - 59 |
11 |
|
6 |
60 - 69 |
3 |
|
7 |
70 - 79 |
1 |
Distribution of cases in various BI-RADS and IAC Code categories
|
BIRAD category |
IAC CODE |
Total | ||||
|---|---|---|---|---|---|---|
|
1 |
2 |
3 |
4 |
5 | ||
|
1 |
0 |
5 |
1 |
1 |
0 |
7 |
|
2 |
1 |
20 |
1 |
0 |
1 |
23 |
|
3 |
0 |
6 |
1 |
0 |
2 |
9 |
|
4 |
0 |
5 |
0 |
3 |
7 |
15 |
|
5 |
0 |
1 |
0 |
0 |
5 |
6 |
|
Total |
1 |
37 |
3 |
4 |
15 |
60 |
Distribution of benign and malignant lesions in Mammography and FNAC
|
Mammography |
FNAC |
Total | |
|---|---|---|---|
|
Benign cases |
Malignant cases | ||
|
Benign cases |
35 |
4 |
39 |
|
Malignant cases |
6 |
15 |
21 |
|
Total |
41 |
19 |
60 |
Association of FNAC findings with histopathology diagnosis
|
FNAC |
HPE |
Total | |
|---|---|---|---|
|
Benign |
Malignant | ||
|
Benign |
12 |
3 |
15 |
|
Malignant |
1 |
14 |
15 |
|
Total |
13 |
17 |
30 |
Sensitivity, Specificity, PPV, NPV and Diagnostic Accuracy of FNAC diagnosis in comparison with Histopathology.
|
Statistic |
Value |
95% CI |
|---|---|---|
|
Sensitivity |
82.35% |
56.57% to 96.20% |
|
Specificity |
92.31% |
63.97% to 99.81% |
|
Positive Predictive Value |
93.33% |
67.77% to 98.95% |
|
Negative Predictive Value |
80.00% |
58.60% to 91.87% |
|
Accuracy |
86.67% |
69.28% to 96.24% |
Association of mammography findings with histopathology diagnosis.
|
Mammography |
HPE |
Total | |
|---|---|---|---|
|
Benign |
Malignant | ||
|
Benign |
10 |
4 |
14 |
|
Malignant |
3 |
13 |
16 |
|
Total |
13 |
17 |
30 |
Sensitivity, Specificity, PPV, NPV and Diagnostic Accuracy of Sono-Mammography using ACR BIRADS for breast lesions in comparison with Histopathology
|
Statistic |
Value |
95% CI |
|---|---|---|
|
Sensitivity |
76.92% |
50.10% to 93.19% |
|
Specificity |
76.47% |
46.19% to 94.96% |
|
Positive Predictive Value |
71.43% |
60.81% to 92.37% |
|
Negative Predictive Value |
81.25% |
50.23% to 86.10% |
|
Accuracy |
76.67% |
57.72% to 90.07% |
Sensitivity, Specificity, PPV, NPV and Diagnostic Accuracy of Sono-Mammography using ACR BIRADS for breast lesions in comparison with FNAC
|
Statistic |
Value |
95% CI |
|---|---|---|
|
Sensitivity |
85.37% |
54.43% to 93.95% |
|
Specificity |
78.95% |
70.83% to 94.43% |
|
Positive Predictive Value |
89.74% |
53.40% to 84.50% |
|
Negative Predictive Value |
71.43% |
78.40% to 95.47% |
|
Accuracy |
83.33% |
71.48% to 91.71% |
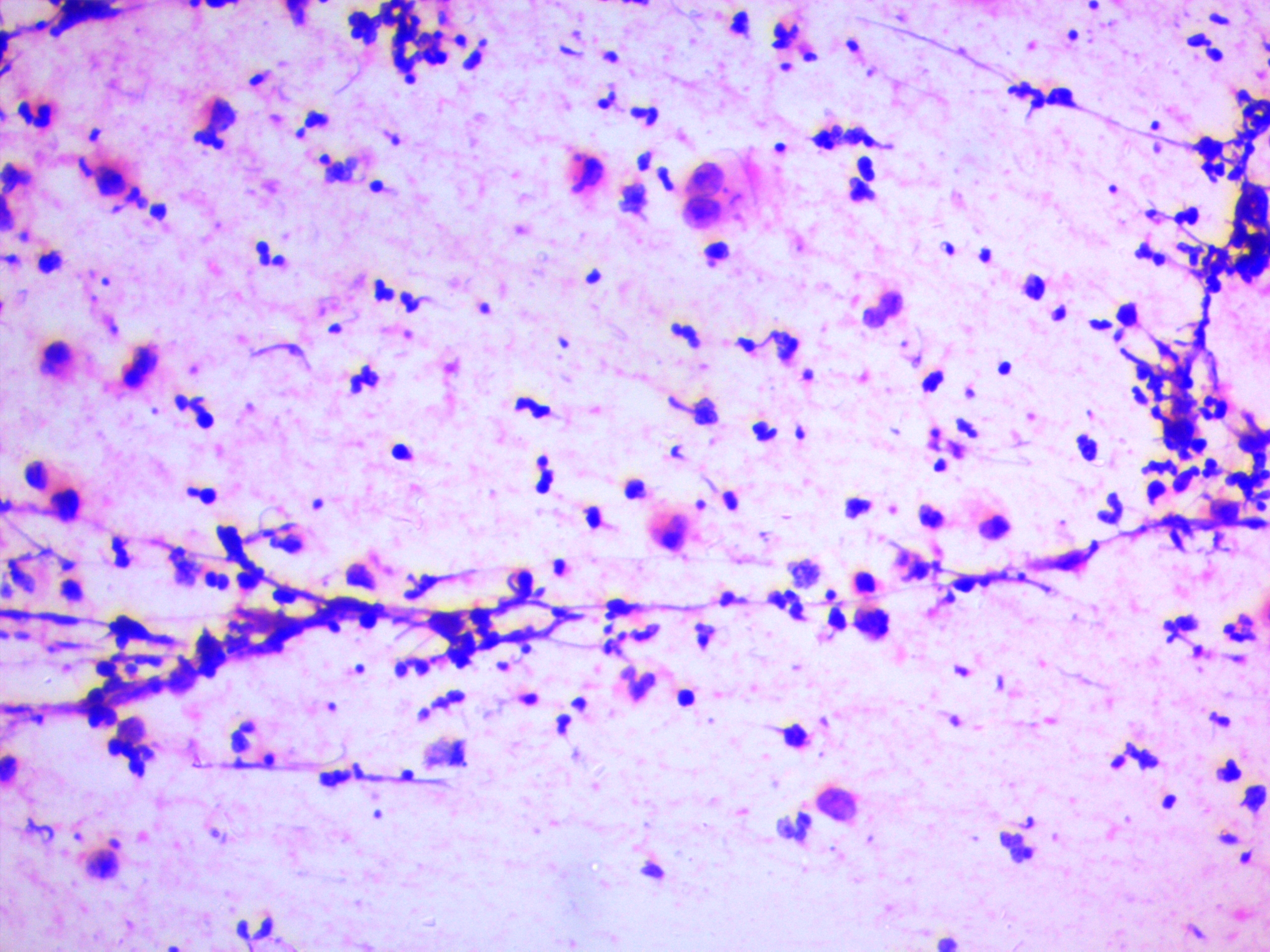
Microphotograph shows inflammatory cells and cyst macrophages. (H&E X400)

Microphotograph shows adipocytes and epithelial cells with atypical nucleus. (H&E X400)

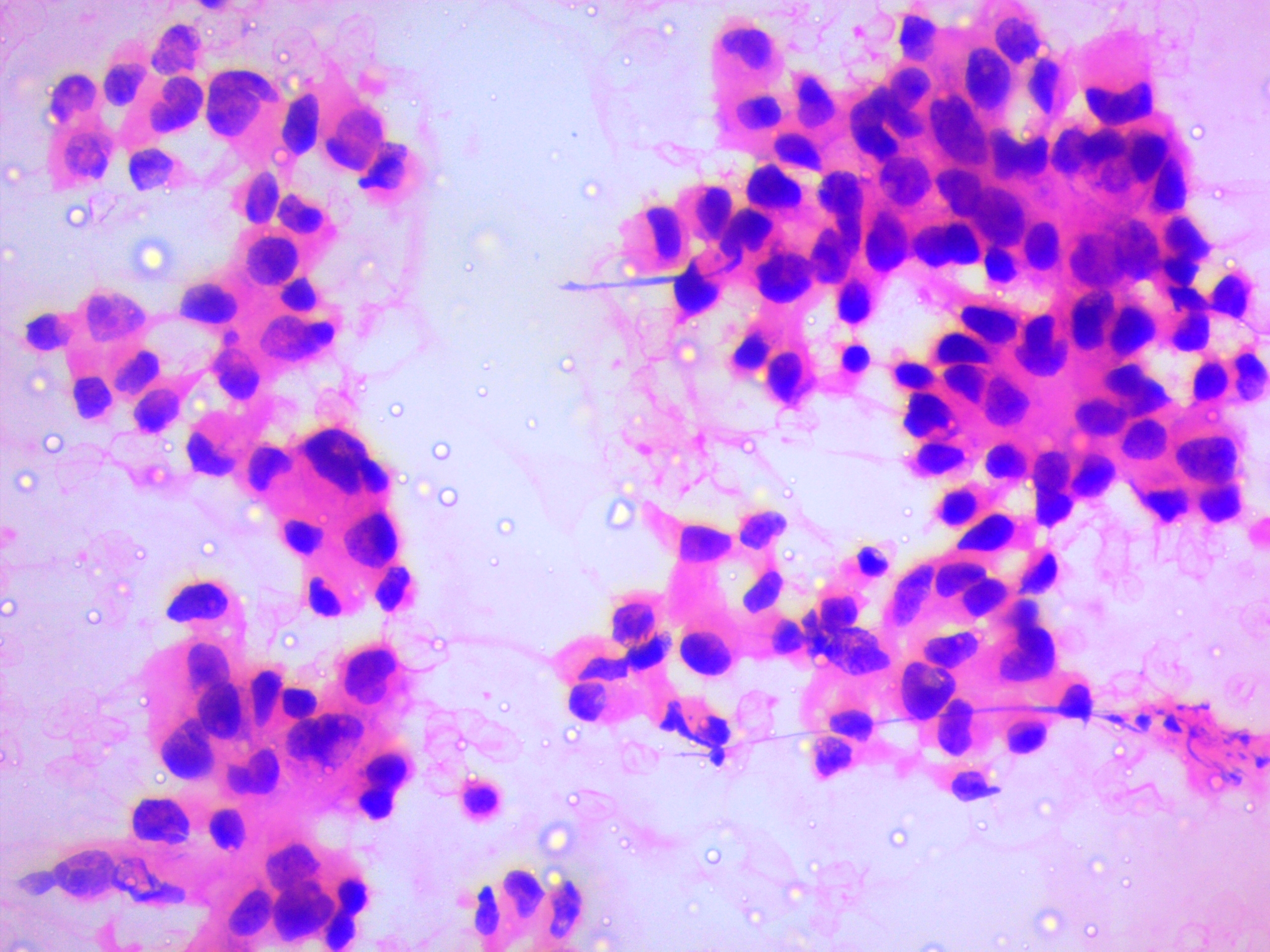
Microphotograph shows high cellularity with atypical ductal epithelial cells in clusters. (H&E X100)
Microphotograph shows highly dysplastic ductal epithelial cells in loose cohesive clusters. (H&E X400)
Results
A total of 60 patients were included in the study. The youngest patient was 16 years of age, while the oldest patient was 75 years of age. The maximum number of cases was seen in the 40–49-year age group. The mean patient age was 40.11 years. Of the 60 patients, 59 were women, and 1 was a man (
On FNAC, there were 41 (68.3%) lesions reported as benign and 19 (31.6%) as malignant. Per the IAC category, 1 (1.6%) patient was categorized under C1, 37 (61.6%) under C2 (Figure 1), 3 (5.0%) under C3 (Figure 2), 4 (6.6%) under C4 (Figure 3), and 15 (25%) under C5 (Figure 4) (
On mammography, there were 39 (65%) lesions reported as benign and 21 (35%) as malignant. No patients scored 0 or 6. In particular, 7 (11.6%) patients scored 1; 23 (38.3%) scored 2; 9 (15%) scored 3; 15 (25%) scored 4; and 6 (10%) scored 5 (
Of all 60 cases, 35 benign cases and 15 malignant cases were concordant with the diagnosis according to the BIRADS score and IAC category. The association between the BIRADS score and IAC category was significant (p = 0.004) (
Discussion
Breast diseases are more common in women than in men. In developing countries such as India, women, especially from rural areas, are usually unaware of breast diseases and are hesitant to discuss/reveal the disease to their family members or family physician. Therefore, breast cancer is generally detected in the advanced stage9. Both the incidence and mortality of this type of cancer are increasing steadily over the past decade10. Breast cancer is the second most common cancer worldwide. The global incidence is 2,088,845 in 201811. In India, the incidence of breast cancer is 25.8 per 100,000 individuals. The incidence in Bangalore is 34.4%, and the prevalence in Kolar is 6.4% among women3.
In the present study, the maximum number of cases was seen in the patients aged 40 – 49 years, with an average age of 41 years. Pandia . and Umat reported that the average age of patients with breast cancer was 50 and 41 years, respectively10, 12. Herein, 15 malignant cases were observed among the patients above 40 years of age, whereas 27 benign cases were noted among those below 40 years of age. The maximum number of discordant cases was observed among the patients below 40 years age.
Of our 60 FNAC-confirmed cases, 41 (68%) were benign, and 19 (32%) were malignant. This is comparable to the findings by Waghmare .: Approximately 56.25% and 31.5% of their cases were benign and malignant, respectively, on FNAC13. Further, Pandia . and Umat reported 55.43% and 38%10 and 55% and 45%12 as benign and malignant cases, respectively. The benign lesions observed in the current study were fibroadenoma, fibrocystic disease, gynecomastia, galactocele, and mastitis. The malignant cases were mainly ductal carcinoma. On FNAC, fibroadenoma (41%) was more common among the benign lesions and ductal carcinoma (92%) among the malignant lesions, comparable with the study findings by Umat 12.
The IAC established a comprehensive and standardized approach to FNAC data reporting. It categorized breast lesion according to the C code. In the present study, the FNAC findings based on the IAC category were compared with the available gold standard histopathological findings. Of the 60 patients, only 30 underwent surgery and histopathological examination. Of the 15 benign cases on FNAC under IAC categories C2 and C3, 12 were benign, and 3 were malignant on histopathology. Of the 15 malignant cases on FNAC under IAC categories C4 and C5, one case reported as suspicious for malignancy on FNAC was benign on histopathology.
Several studies have compared the overall diagnostic accuracy of FNAC with respect to histopathology of palpable breast lesions. In the study by Rahman ., the diagnostic sensitivity, specificity, PPV, NPV, and accuracy were 97.2%, 99.46%, 97.2%, 99.4%, and 99.9%, respectively14. In the study by Choi ., the diagnostic sensitivity, specificity, PPV, NPV, and accuracy were 77.7%, 99.2%, 88%, 98.4%, and 91.1%, respectively15. Sankaye . reported a diagnostic sensitivity, specificity, PPV, NPV, and accuracy of 88.37%, 96.42%, 84.37%, 97.43%, and 91.54%, respectively16. Bhukari demonstrated a diagnostic sensitivity, specificity, PPV, NPV, and accuracy of 98%, 100%, 97%, 100%, and 98%, respectively17. In the present study, a sensitivity of 82.35%, a specificity of 92.31%, a PPV of 93.3%, an NPV of 80%, and an accuracy of 86.67% were noted. This difference among various studies may be attributed to the use of blinded (unguided) FNAC, which might have missed the exact site of lesions.
Patients with palpable breast lesions commonly present to clinics/hospitals for radiological evaluation. Mammography is the preliminary method of diagnosis, with a sensitivity of 85 — 95%. The sensitivity of mammography in the diagnosis of breast lesions widely varies from 67% to 97%. The rate of false-negative findings is high at 4 — 12%9. Herein, the sensitivity of mammography was 76.47%, and the false-negative rate was 18%.
Numerous studies have reported the overall accuracy of mammography (BIRADS score) compared with that of histopathology of palpable breast lesions. In the study by Rahman ., the diagnostic sensitivity, specificity, PPV, NPV, and accuracy were 82.76%, 90.36%, 75%, 93.7%, and 88.39%, respectively14. Tiwari . reported sensitivity, specificity, PPV, and NPV of 77.7%, 97.72%, 87.5%, and 95.5%, respectively18. Bak . demonstrated sensitivity, specificity, PPV, and NPV of 91%, 88%, 96%, and 71%, respectively19. The present study showed similar results: sensitivity of 76.92%, specificity of 76.47%, PPV of 71.43%, NPV of 81.25%, and accuracy of 76.67%.
Herein, four discordant cases reported as benign on mammography were malignant on FNAC, while six discordant cases reported as malignant on mammography were benign on FNAC. The association between the BIRADS score and IAC category was significant (p = 0.004). This result is similar to the p value (0.001) reported by Bak 19.
Various studies have demonstrated the overall accuracy of mammography (BIRADS score) compared with that of FNAC of palpable breast lesions. Pandia . reported a diagnostic sensitivity, specificity, PPV, NPV, and accuracy of 88.57%, 82.46%, 75.61%, 92.16%, and 84.78%, respectively10. In the study by Rathi, the diagnostic sensitivity, specificity, PPV, NPV, and accuracy were 84.21%, 97.73%, 94.12%, 93.48%, and 93.65%, respectively20. Navya . showed a diagnostic sensitivity, specificity, PPV, NPV, and accuracy of 88%, 87.5%, 80%, 93%, and 88%, respectively9. The present study demonstrated similar results: sensitivity of 85.37%, specificity of 78.95%, PPV of 89.74%, NPV of 71.43%, and accuracy of 83.33%.
The limitation of the present study was that it was conducted at a single center and had a small sample size. Only 30 cases had available histopathological findings. Hence, further multicentric studies with larger sample sizes are needed for better utilization of mammography and FNAC to diagnose breast lumps early and plan appropriate treatment. Nevertheless, the present findings suggest that mammographic, FNAC, and histopathological findings are all notable.
Conclusions
FNAC with IAC category assessment and mammography with BIRADS scoring can be used as first-line diagnostic tests for breast lumps. However, FNAC is more sensitive in diagnosing breast lumps than mammography.
Abbreviations
BIRADS: Breast imaging reporting and data system, FBAC: Fine needle aspiration cytology, IAC: International academy of cytology, NPV: Negative predictive value, PPV: Positive predictive value, SPSS: Software package for social sciences
Acknowledgments
None.
Author’s contributions
SD: Data collection, manuscript writing, manuscript editing; KR: Concept, manuscript writing, manuscript editing, manuscript reviewing; AT: Data collection, manuscript writing; AKS: Manuscript editing; SPN: Manuscript reviewing. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The institutional review board approved the study, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.

