D4 Duodenal Injury and Literature Review: A Case Report
- Department of Gastrointestinal and Hepatobiliary Surgery, Thai Nguyen National Hospital, Thai Nguyen, Viet Nam
- Oncology department, Viet Duc University Hospital, Ha Noi, Viet Nam
- Department of Otorhinolaryngology, Thai Nguyen National Hospital, Thai Nguyen, Viet Nam
- Department of Tropical Medicine, Thai Nguyen National Hospital, Thai Nguyen, Viet Nam
Abstract
This article has been retracted by the authors.
Introduction: Duodenal injury from blunt abdominal trauma is rare and often requires complex repair methods. We report a case that was successfully managed with primary repair plus feeding jejunostomy. We also reviewed the literature on fourth-portion (D4) duodenal injuries.
Case presentation: A 34-year-old man presented to the emergency department after a workplace accident with severe epigastric pain. His vital signs were stable. Abdominal examination revealed marked tenderness, bruising, superficial abrasions, generalized rigidity, and absent bowel sounds. Computed tomography of the abdomen showed free air in the peritoneal and retroperitoneal spaces. Four hours after injury, the patient underwent emergency laparotomy. We identified ruptures of the fourth portion of the duodenum and the stomach. Both defects were closed primarily, and a feeding jejunostomy was created. The postoperative course was uneventful.
Clinical discussion: Rupture of the D4 segment can result from a fall onto the back, whereas gastric rupture often follows direct anterior impact. Free retroperitoneal air adjacent to D4 strongly suggests duodenal injury. We mobilized the surrounding tissue and performed a two-layer repair, supplemented by feeding jejunostomy to reduce the risk of duodenal leakage.
Conclusion: Primary repair accompanied by wide abdominal drainage and feeding jejunostomy is a simple, safe, and effective option for uncomplicated D4 duodenal injuries.
Introduction
Duodenal injury from blunt abdominal trauma is rare, with an estimated incidence of 3–5 % among patients with abdominal trauma1. These injuries are often severe, with reported mortality rates ranging from 0 to 9.5%1, 2. In the past in our country, complex repair methods—such as duodenal diverticulization, pyloric exclusion with gastrojejunostomy, pancreaticoduodenectomy, and duodenojejunostomy—were preferentially used to manage duodenal injuries1, 3. However, recent studies indicate that primary repair is becoming the preferred treatment, as it shortens operative time, hospital stay, complication rates, and postoperative mortality1, 4.
The duodenum is divided into four sections (D1–D4), of which the fourth segment (D4) is the least commonly injured in blunt abdominal trauma5. Because D4 is relatively mobile, readily accessible, and less intimately associated with the pancreatic head and biliary tree than D1 or D2, injuries at this site are generally less complex and amenable to simpler repair3.
We present a case of a D4 duodenal injury concomitant with a gastric laceration that was successfully managed with primary repair and a feeding jejunostomy. Through this case, we aim to provide clinicians with an additional, less invasive option for repairing D4 duodenal injuries. This report was prepared in accordance with the SCARE 2023 guidelines6.
Case presentation
Patient information
A 34-year-old male presented to the emergency department with severe abdominal pain following a workplace accident. Approximately 1 hour before admission, the patient had fallen backward while climbing a ladder and had been struck directly in the epigastric area by a heavy object. After the accident, he awoke with no memory loss and immediately experienced severe abdominal pain and dizziness without dyspnea or chest pain. The patient was transported to Thai Nguyen National Hospital in Vietnam by family members. Upon arrival, his condition was assessed according to the Advanced Trauma Life Support algorithm. The airway was patent and bilateral breath sounds were clear. Heart rate was 91 beats per minute, blood pressure 130/80 mmHg, and respiratory rate 19 breaths per minute. He was conscious and lucid, with no neurologic deficits. He had no significant medical history or known drug allergies.
Abdominal examination revealed severe pain, bruising, and skin abrasions in the epigastrium (≈ 3 × 5 cm), accompanied by guarding and absent bowel sounds. Lumbar examination showed mild pain without bruising, normal limb movement, and no suspicion of spine injury. Blood tests demonstrated a white-blood-cell count of 16.49 × 10⁹/L; lipase, amylase, and other parameters were within normal limits. A Focused Assessment with Sonography for Trauma (FAST) examination detected a small amount of free fluid in Morison’s pouch, around the spleen, and in the Douglas pouch, with no solid-organ injury. Contrast-enhanced computed tomography (CT) of the abdomen revealed free air in the peritoneal and retroperitoneal spaces, a small volume of free fluid, soft-tissue infiltrates, and air bubbles adjacent to D4 (Figure 1). Chest radiography was normal and showed no spinal injury.
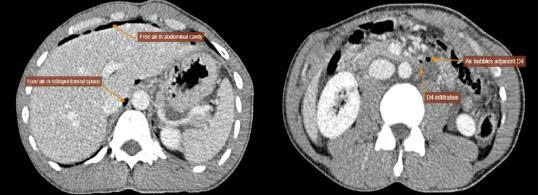
Axia contrast-enhanced abdominal CT scan demonstrating free intraperitoneal air (white arrow) and retroperitoneal air (asterisk) adjacent to the fourth part of duodenum (D4). Note the infiltration and air bubbles (black arrow) near D4, suggestive of duodenal perforation.
Pre-operative diagnosis and prognosis
Based on clinical findings, the patient exhibited peritoneal signs requiring surgery, together with CT evidence of free intraperitoneal and retroperitoneal air without solid-organ injury. A preliminary diagnosis of hollow-viscus perforation secondary to blunt abdominal trauma was made. The presence of retroperitoneal air and infiltration around D4 suggested a duodenal injury, considered a poor prognostic indicator.
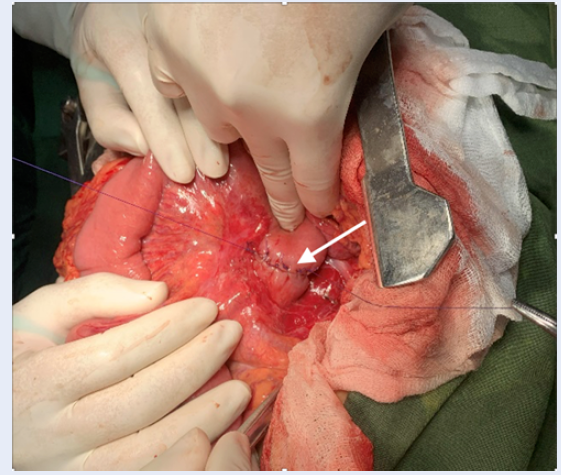
Intraoperative photograph (anterior view) showing a 3x5 cm full thickness rupture (arrows) along the lesser curvature of the stomach. The edges of the defect are clean without signs of ischemia.
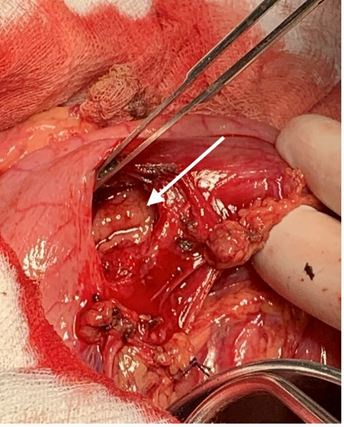
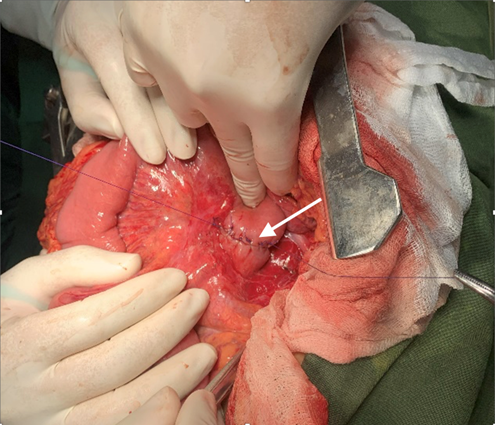
Intraoperative photograph (retroperitoneal view) of the fourth part of the duodenum (D4) after mobilization of the ligament of Treitz, revealing a circumferential rupture involving 40% of the duodenal wall (arrows). The wound edges are viable and non-contuse.
Surgical intervention
Laparotomy was performed 3 hours after arrival. A midline incision (~ 20 cm) extending above and below the umbilicus was used. A large volume of digestive fluid was found in the peritoneal cavity. The lesser curvature of the stomach had a 3 × 5 cm rupture (Figure 2). After a Kocher maneuver, the pancreas and D1–D3 segments of the duodenum were intact, but the fourth part (D4) was lacerated along approximately 40 % of its circumference, with sharp, non-crushed edges (Figure 3).
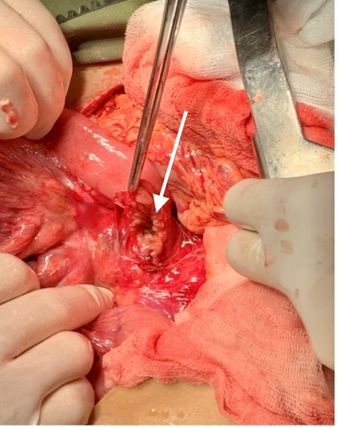
No additional intra-abdominal injuries were identified. The gastric defect was debrided and closed in two layers. At the duodenal site, the Treitz ligament was divided, and D3–D4 were mobilized to expose the lesion. The wound edges were debrided and sutured in two layers (Figure 4). Approximately 40 cm distal to the duodenal repair, a feeding jejunostomy was created. The peritoneal cavity was irrigated with 0.9 % saline. Two F16 drains were placed beneath the duodenal repair and two F16 drains in the Douglas pouch; a nasogastric decompression tube was also inserted.
Intraoperative photograph following two-layer primary repair of the D4 duodenal rupture. The sutured site (arrows) shows tension-free closure with intact serosal integrity.
Results
Nutrition was provided via jejunostomy for the first 10 post-operative days. The nasogastric tube was removed and oral feeding began on post-operative day 11. Clinical status and laboratory tests remained normal. The patient experienced no complications and was discharged home after 13 days.
Discussion
Duodenal injuries, although rare, are associated with high mortality and complication rates2, 7. Because of their rarity, clinicians may overlook them after blunt abdominal trauma, leading to delayed diagnosis and serious consequences.
AAST Duodenal Injury Classification
The American Association for the Surgery of Trauma (AAST) classifies duodenal injuries into five grades (I–V) based on damage to the duodenum and adjacent organs (pancreas, extrahepatic biliary tree). This standardized grading guides treatment selection and prognostication8.
Diagnosis
Multi-detector CT focused on the pancreas and duodenum is the primary imaging modality for suspected duodenal injury. Characteristic findings include retroperitoneal free air, duodenal wall laceration or thickening, and periduodenal hematoma7, 9. Our patient sustained a direct epigastric blow and exhibited peritoneal signs. CT demonstrated intraperitoneal and retroperitoneal free air, air bubbles around D4, and disruption of the gastric curvature, prompting a pre-operative diagnosis of hollow-viscus perforation and immediate surgery. Nevertheless, many patients with duodenal injuries present with nonspecific symptoms that hinder early detection. E. G. Santos highlights the pivotal role of understanding the mechanism of injury—such as a high fall onto the back or a direct epigastric impact—in guiding diagnostic work-up10. If clinical suspicion persists, CT or MRI of the duodenum should be performed to secure an early diagnosis7, 10.
Management
During laparotomy for blunt abdominal trauma, the surgeon first controls hemorrhage and then assesses visceral injuries7, 11. Systematic exploration, including a Kocher manoeuvre, exposes the duodenum’s anterior and posterior surfaces. D4 is inspected after division of the ligament of Treitz with careful protection of neighbouring vessels7. Intra-operative findings are graded according to the AAST classification12.
Treatment depends on injury site, AAST grade, and the patient’s physiological status7, 12. Options range from simple primary closure to complex procedures such as pancreaticoduodenectomy, duodenal diverticulisation, Roux-en-Y duodenojejunostomy, or triple-tube ostomy. Primary repair is now favoured for Grade I–II injuries1, 2, 7, 13. For Grade III–IV lesions, feasibility of primary repair hinges on timing, tissue viability, and associated injuries1, 3, 7. Grade IV–V injuries frequently involve severe pancreatic damage; most authors recommend complex reconstruction owing to high leak and mortality rates12, 14.
Surgical procedure
Our patient had a Grade II laceration involving <50 % of the circumference of D48. Degiannis regards D3-D4 as the distal duodenum and treats lesions there in a manner analogous to small-bowel injury3.
The optimal management of duodenal trauma remains debated and is often influenced by surgical experience. R.D. Weale reported successful primary repair for Grade I–III injuries throughout the duodenum, concluding that the shift toward simple closure is warranted, although Grade III lesions, delayed presentation, or contaminated fields carry an increased leak risk4. J.M. Aceves-Ayala likewise supports primary repair for all Grade I–II injuries and selected Grade III defects; delayed or heavily contaminated Grade II lesions should be treated as Grade III, occasionally necessitating Roux-en-Y duodenojejunostomy15. Collectively, these data endorse primary repair for D3–D4 injuries up to Grade III3, 4, 15.
Because the risk of leakage was uncertain, we placed a feeding jejunostomy and wide drainage. Early enteral nutrition likely contributed to the patient’s uneventful recovery. Dickerson. demonstrated that early postoperative feeding reduces complications and mortality in severe duodenal trauma16. Current literature therefore recommends feeding jejunostomy, especially for high-grade injuries7, 17. Adequate external drainage permits early detection and control of leaks, creating a manageable fistula if necessary. Early enteral support also prevents electrolyte disturbances and malnutrition when oral intake is delayed by fistula formation.
This report supports the feasibility and safety of uncomplicated D4 primary repair and offers an illustrative example for settings with limited resources. While encouraging, our conclusions are based on a single case and therefore require validation in larger series.
Conclusions
Our case report demonstrates that primary repair, supplemented with extensive abdominal drainage and a feeding jejunostomy, is a feasible and effective method for treating uncomplicated D4 duodenal injuries. This finding supports the utility of primary repair as a viable option for selected cases—particularly those without significant tissue loss or other complications—offering a less complex yet effective management strategy. Clinicians confronting similar rare injuries should consider this approach, as it can yield favorable outcomes and expedite recovery, even in resource-constrained settings.
Abbreviations
AAST: American Association for the Surgery of Trauma, CT: Computed Tomography, D4: Fourth portion of the Duodenum, FAST: Focused Assessment with Sonography for Trauma, MRI: Magnetic Resonance Imaging, SCARE: Surgical CAse REport guidelines
Acknowledgments
None.
Author’s contributions
S.T.D.: Concept and design, data interpretation and analysis, drafting, revision, and approval of final manuscript. S.H.T and H.D.H: Design, data collection, data interpretation and analysis, drafting, revision, and approval of the final manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data availability statement: The data that support the findings of this case report are available upon reasonable request from the corresponding author, with appropriate ethical considerations for patient privacy.
Ethics approval and consent to participate
Ethical approval was waived by the institutional policy of Thai Nguyen National Hospital for retrospective case reports that do not involve identifiable patient information or interventions. Decision No. 478/qd-bv Dated February 24, 2024
Consent for publication
Written informed consent was obtained from the patient’s mother for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Declaration of generative AI and AI-assisted technologies in the writing process
The authors declare that they have used generative AI and/or AI-assisted technologies in the writing process before submission, but only to improve the language and readability of their paper.
Competing interests
The authors declare that they have no competing interests.

